Osteoporosis is a condition where loss of bone develops to the point where our bones break easily. It is a serious condition that increases slowly as we age. Generally osteoporosis is asymptomatic (we are unaware that we have it) until there is a fall or injury resulting in a fracture. We all get osteoporosis as we age so it is important that we learn about it and try to do something to slow it down or reverse the process.
Common areas of the body where osteoporosis fractures occur:
- the wrist - usually following a fall on the outstretched hand
- the hip - often from slipping and twisting during a fall
- the spine - from bending forward or heavy lifting
Bone tissue is a rigid, living structure that is constantly renewing itself. It is not an unchanging skeleton made of calcium. Microscopic holes are constantly created by bone eating cells called osteoclasts. Once these bone cavities are created, bone building cells called osteoblasts form new bone. This process rejuvenates the bone and repairs any damage.
In early childhood and adolescent years our bones grow rapidly. Good dietary calcium intake and regular exercise in these formative years are important for good bone health and peak bone mass. Bones may reach their mature length or height in the late teens but bone density and strength continue to build along with body weight and muscle strength into one's 20s and possibly 30s.
After you've reached your peak bone mass in your 30s, your body will replace old bones at the same rate that new ones are produced. Starting in your 40s, your bones will start to break down faster than they can be replaced. In women, the hormone estrogen contributes to the bone-building process, so as estrogen levels fall when women approach menopause, the bone loss rate accelerates. Women can lose 40% of their inner bone mass and 10% of their outer bone mass within the 10 years after menopause. This makes it particularly important to increase your intake of vitamin D and calcium, and explore other treatments such as with calcitonin and biophosphonates.
As we approach our later decades of life, many changing conditions make us more susceptible to fractures related to osteoporosis. The most important of these are decreased bone strength and increased risk of falls.
We are more likely to fracture a bone as we get older because of these reasons:
- decreased bone strength due to reduced bone density
- increased tendency to fall due to:
- reduced muscle strength so we are less likely to break a fall
- decreased vision, making it more likely for us to trip
- poor balance mechanism making us more unsteady on our feet
- posture changes resulting in center of gravity changes and more sway as we walk
- changes in blood pressure or heart rate resulting in dizziness and unpredictable falls
- medications that result in weakness or lightheadedness
Obviously, efforts should be made to minimize osteoporosis fractures before they happen. Physicians can identify individuals at high risk of osteoporotic fractures by doing a bone density test. It is also important to investigate whether the person is at a higher risk than normal for falling, especially if something can be done to reduce that risk.
All material copyright MediResource Inc. 1996 – 2024. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Learn-About-Osteoporosis
All of us will get osteoporosis if we live long enough. Since none of us have a crystal ball to predict our life expectancy, we should all do our best to ensure good strong bones and prevent falls no matter how long we live.
Osteoporosis is extremely common. It is estimated that at least 1 in 3 women and 1 in 5 men will break a bone in their lifetime if they have osteoporosis. Osteoporosis causes 70% to 90% of the 30,000 hip fractures that occur every year in Canada. Men typically have a higher peak bone mass, so it takes longer for bone loss to reach a level where the bones fracture. Nevertheless, as men increasingly live past age 80, osteoporosis is going to become a more common problem for men.
Research has identified a number of risks that make it more likely for one individual over another to get osteoporosis.
If several of these risk factors apply to you, you may want to check with your doctor about how to prevent osteoporosis.
Risk factors for osteoporosis we cannot change:
- genetics (family history)
- female sex (osteoporosis affects women more than men)
- age (even if we keep saying we are 39, our bone mass decreases with age)
Lifestyle risk factors for osteoporosis we can change:
- low dietary calcium and vitamin D
- smoking
- excess alcohol use (more than 3 drinks per day)
- excessive emotional stress
- possible excess caffeine
- weight loss greater than 10% since age 25
Medical conditions and diseases that increase risk of osteoporosis:
- neurological disorders (e.g. Parkinson's disease, multiple sclerosis)
- malabsorption syndromes (e.g. Crohn's disease, ulcerative colitis)
- thyroid disease (overactive thyroid or excess thyroid supplements)
- long-term synthetic glucocorticoid (e.g. prednisone, dexamethasone) use
- anticonvulsants (seizure medications)
- liver or kidney disease
Medical conditions in women:
- estrogen deficiency (surgical removal of ovary)
- early menopause (before age 45)
- exercise-induced absence of menstrual periods (seen in high performance athletes)
Medical conditions in men:
- testosterone deficiency (gonadal or testicular failure) measured by an early morning testosterone level (blood test)
If you find that a number of these risks apply to you, you may want to think about making some simple changes in lifestyle, doing a test for osteoporosis or even starting medications that are available.
The risk factors of family history, female sex, and advancing age are powerful predictors of osteoporosis.
If you have these risks, then a bone density test can more accurately predict if osteoporosis is present.
Your other risk factors for osteoporosis should be assessed as well. Each added risk factor contributes towards the suspicion of osteoporosis. One or more risk factors might be reason enough to proceed to a bone density test.
All material copyright MediResource Inc. 1996 – 2024. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Learn-About-Osteoporosis
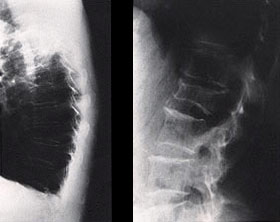
Osteoporosis should be suspected in any individual who has a fracture. X-rays will usually confirm a fracture if there is one. X-rays should be done if a limb or other bone is acutely painful after a fall or injury. Sometimes individuals will have mild to severe chronic back pain, and X-rays of the thoracic or lumbar spine might detect a wedge or crush fracture (see Figure 1). Any individual with a significant fracture needs to be assessed to exclude or identify medical problems that could have played a role in the resulting fracture.
Individuals who have not had any fractures but do have a number of risk factors for osteoporosis need an examination called a bone density test to determine if osteoporosis is present.
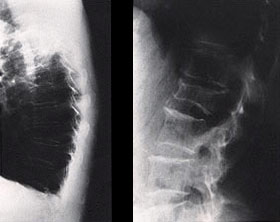
Figure 1
A lateral X-ray of the thoracic spine (left) might reveal small wedge fractures, or of a lumbar spine (right) might reveal a more significant crush fracture.
What is a bone density test?
A bone density test determines the bone mineral (calcium) content of certain bones. It is a simple, painless procedure that can measure the calcium content of bones in specific body areas including the spine, hip, forearm, or total body. The most common bone density test used to diagnose and monitor osteoporosis is dual-energy x-ray absorptiometry (DXA).
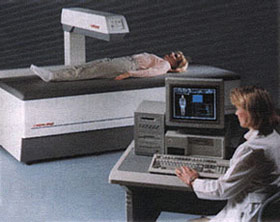
During the DXA bone density test (see Figure 2), the individual lies perfectly still on a special table while a mechanical arm passes over the body. The mechanical arm sends an X-ray beam through the bones being scanned. A detector arm below the body determines how much of the X-ray beam passes through the body and, from that measurement, calculates how much bone is present. That calculation is then compared with the average for men and women of the same sex and age. Your doctor will discuss the results of the bone density test and help you make a decision about treatment options.
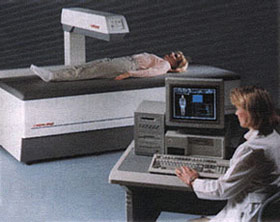
Figure 2
A DXA bone density test can be done quickly and in comfort.
The radiation risk is minimal - a single bone density test gives about one-tenth the radiation as a chest X-ray. This is the same radiation exposure as you receive flying from the east coast to the west coast of North America. Nevertheless, a woman should not have a test if she is pregnant.
It might be recommended to repeat a bone density test to make sure there is not further bone loss over time or to help evaluate if the treatment is effective. Generally a repeat bone density in 1 to 3 years is sufficient to see if there has been a significant change in bone density.
Figure 3
A T-score gives you a good idea of how strong your bones are now compared with what they were at their strongest. It does this by comparing current bone density with peak bone density. A T-score of -2.5 often indicates osteoporosis.
Who should get a bone density test to diagnose osteoporosis?
Osteoporosis Canada has set clear guidelines on deciding who should get bone density testing. It is recommended that all individuals over 65 or younger individuals with risk factors for fractures or low bone mass should receive a bone density test.
How do you interpret the results of a bone density test?
An individual's bone density result is compared with the average for individuals of the same age and sex. Your doctor will explain the results. Often, the result of the test is reported as a T-score. A T-score is a measure of your current bone density compared with what the density theoretically was at its peak (see Figure 3).
All material copyright MediResource Inc. 1996 – 2024. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Learn-About-Osteoporosis