Description of the test
Spirometry, also known as lung function tests or pulmonary function tests, is a quick and painless diagnostic procedure used to evaluate lung function. Spirometry is typically used when your doctor suspects chronic obstructive pulmonary disease (COPD), asthma, or if you have undiagnosed respiratory symptoms such as wheezing, coughing, or shortness of breath.
This simple procedure may be performed in your doctor's office or by a specialist at a local pulmonary function laboratory. Your health care provider will have you breathe slowly, normally, or forcefully into a device known as a spirometer to assess your lung function by taking several different measurements.
Once completed, your health care provider will interpret your spirometry results by comparing it to normal values obtained from individuals with healthy lungs, while taking into account variables that can influence results such as your age, height, gender, and ethnic group.
If your values are below the lower limit of normal (LLN) of what is predicted, then you may have some form of chest or lung disease.
How often should the test be performed?
Your doctor will recommend when and how frequently this test is required.
Why is this test performed?
Spirometry is used to help confirm whether or not someone has a lung condition. It is especially useful for diagnosing COPD or asthma. Both COPD and asthma are known as obstructive lung diseases because conditions such as inflammation in the lungs or the passageways leading to the lungs obstruct air flow to and from the lungs.
Spirometry can also be used to determine if the lung condition is progressing or to see if medical treatment is helping to relieve symptoms of the condition.
Are there any risks and precautions?
Spirometry is safe, but there are some situations where it might be advisable to delay testing or seek expert advice. These include:
- a known or suspected ongoing respiratory infection
- hemoptysis (coughing up blood) of unknown origin
- pneumothorax (collapsed lung)
- unstable cardiovascular status including recent heart attack, uncontrolled high blood pressure, or pulmonary embolism (blood clot in lung)
- history of hemorrhagic cerebrovascular event (e.g., a stroke)
- recent chest, abdominal, or eye surgery
- nausea, vomiting, or pain
- confusion, dementia
- less than 5 years of age
Tell your doctor if any of these apply to you. If you are concerned about any symptoms following this test, speak to your doctor.
Take the time to be sure you understand all the risks of complications and side effects as well as any precautions that you or your doctor can take to avoid them. Be sure your doctor understands all your concerns.
What happens during the test?
Spirometry is a quick and painless procedure usually performed in a doctor's office or a specialized pulmonary function laboratory. Your height, weight, age, and gender will be recorded as they are known to affect spirometry results.
During a spirometry test, you will be sitting down and will be asked to breathe into a mouthpiece connected to a spirometer while either pinching your nose closed or wearing a nose clip.
There are many different types of spirometers available and you may find yourself breathing into a small handheld apparatus or a large high-tech machine. Depending on the intended measurement, you may be asked to breathe slowly, normally, or forcefully. You will also be asked to reproduce each breathing exercise several times to ensure accuracy of the measurements.
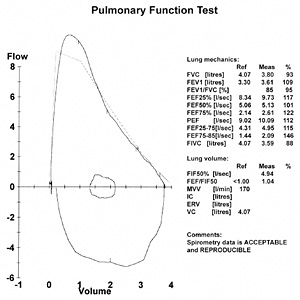
The following are measurements that may be included in your spirometry testing:
- The total amount of air you can forcibly blow from your lungs and the time it takes to perform this task, known as forced vital capacity (FVC) and forced expiratory time (FET), respectively.
- How much air you can blow from your lungs in one second, known as forced expiratory volume in one second (FEV1).
- The total amount of air you can slowly blow from your lung, known as slow vital capacity (SVC).
- The total amount of air you can breathe in, known as inspiratory vital capacity (IVC).*
- The amount of air left in your lungs after a full expiration, known as residual volume (RV).*
*Performed at a lung function laboratory.
If your doctor is not sure whether you have COPD or asthma, you may be asked to have a spirometry test before and after inhaling a bronchodilator, a medication that helps open up the airways to your lungs.
Asthma is known as a reversible obstructive airway disease because the symptoms can be reversed with inhalation of bronchodilator medication. If your spirometry results do not improve significantly with use of the asthma medication, then you likely have a condition such as COPD where the lungs are damaged and not as responsive to bronchodilators (i.e., irreversible obstructive disease).
If your doctor suspects you have asthma but your spirometry tests are normal, you may be asked to use a spirometer before and after a methacholine challenge test. Methacholine is a substance that is used to intentionally trigger asthma symptoms. Additionally, a methacholine challenge can help determine how severe your asthma is by the response of your lungs, as measured by spirometry.
How should I prepare for this test?
You should not eat a heavy meal or have food or drinks with caffeine before the test, or wear tight, restrictive clothing during the test. Smokers should abstain for 4 to 6 hours before the test.
Tell your health care provider prior to the test of any prescriptions, over-the-counter (non-prescription), and herbal medications that you are taking. Also tell them about any medication allergies and medical conditions that you may have. Ask your doctor or pharmacist whether you need to stop taking any of your medications before the test. Depending on why you are having the test, your doctor may ask you not to use one or more of your inhaled medications for a period of time before the test is conducted.
Lastly, emptying your bladder prior to the test is recommended as a full bladder or stress incontinence may cause underperformance in spirometry.
What can I expect after the test?
After this test, you may temporarily feel a little dizziness or lightheadedness from breathing forcefully into the spirometer.
Results
The results of your spirometry test will be compared to reference values that are appropriate for your age, height, gender, and ethnicity. Your doctor will discuss your results with you.
One of the main values analyzed and discussed will be the FEV1/FVC ratio, which for the normal population is typically greater than 0.80 in adults and even higher for children. An FEV1/FVC ratio less than 0.80 suggests airflow obstruction.
For COPD, the Canadian COPD guidelines specify that a FEV1/FVC ratio that is less than 0.70 after administration of a bronchodilator indicates COPD.
FEV1 values alone are used to categorize the severity of airway obstruction that you may have:
- mild, at least 80% of predicted FEV1
- moderate, 50% to 80% of predicted FEV1
- severe, 30% to 50% of predicted FEV1
- very severe, less than 30% of predicted FEV1
FEV1 is also used to confirm the presence of asthma by one of the following criteria:
- an improvement in FEV1 of at least 12% and at least 200 mL, after administration of an inhaled bronchodilator or after a course of therapy using controller medications
- a decline in FEV1 of at least 10 to 15% after exercise
Other spirometry-based measurement such as vital capacities (VCs), residual volumes (VC), and total lung capacity (TLC) can be used to identify other potential sources of lung performance dysfunction, which will likely require further diagnosis.
All material copyright MediResource Inc. 1996 – 2024. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/procedure/getprocedure/Lung-Function-Tests