Avoiding indoor allergens
Minor Ailments
For some people, allergy season lasts all year and its symptoms strike close to home. It can be challenging to avoid your allergy triggers when they're all over your house, but it can be done.
Deal with dust. Keep the house as dust-free as possible. When dusting, use a damp cloth. The dust will cling to the cloth better this way, keeping it from floating off into the air. Regularly wash bedding linens in hot water, and choose sturdy but lightweight fabric blankets that can withstand weekly washings.
The vacuum may seem like an ally to those with allergies, but older vacuums can actually stir up dust. If you can, either wear a protective face mask or find a newer model vacuum with a high efficiency particulate air filter, better known as a HEPA filter. Also, remember to routinely change the vacuum dust bags or clean the dust collector. If all else fails, ask someone else to vacuum for you.
Smooth the surfaces. Dust clings to random clutter like clothes, books, and paperwork. Piles of pillows may please the eye, but they're dust collectors, too, as are stuffed toys. Houseplants seem like they would be good for the air, but they tend to accumulate dust and mould.
You can regularly wipe down surfaces to get rid of dust, but you can also simply reduce the number of dust-gathering surfaces in your home. Opt for hardwoods or linoleum over carpet and rugs, and choose window shades instead of heavy fabric curtains or dust-catching blinds.
Minimize the mould. A cool, well-ventilated home with low humidity levels will invite less mould. Closed-in spaces such as closets, basements, and especially bathrooms are mould magnets. Shower curtains tend to get mouldy after repeated use and should either be regularly bleached or simply replaced.
Protect yourself from pet dander. Unfortunately, most experts would recommend removing allergy-causing animals from the house. You may also want to consider implementing a strict "No pets allowed" policy in bedrooms. Another option is to adopt a hypoallergenic pet that is less likely to cause allergic reactions.
All material copyright MediResource Inc. 1996 – 2026. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Allergy-Prevention-and-Treatment
Avoiding outdoor allergens
Minor Ailments
Pollen plays such a pivotal role in the cycles of the natural world. Pollen causes the telltale seasonal shifts in plants, grasses, and weeds. Pollen also causes the telltale seasonal allergy symptoms so many people suffer from at various times throughout the year.
How can a person prone to seasonal allergies coexist with nature without sneezing, sniffling, and coughing?
Know your triggers. Pollen is the number one culprit in most outdoor seasonal allergies, but pollen from where? Tree pollen causes most springtime symptoms, and the pollen from grasses and weeds set off summer and fall sneezing fits.
Leave pollen where it belongs. Pollen is not as sticky as some allergens but it can come into your house in the air; on your clothes, skin, and hair; and on the fur of pets. Keep the windows closed during allergy seasons, and regularly clear out air filters and air ducts. After being outside in "danger" zones, remove any shoes and clothing that may have gotten soiled with pollen. Take a shower, or at least wash your hands and rinse out your eyes and nose.
Sidestep your triggers. Nature doesn't have to be your enemy! Try to minimize your exposure to your known allergy triggers and if you have seasonal allergies, make the best of the times of the year when you're not suffering from allergy symptoms. For example, if you're allergic to spring tree pollen, save campouts and picnics for late summer or early autumn. If autumn ragweed stuffs you up, make spring your hiking season.
Watch the weather. Pollen is the substance that plants such as trees, weeds, and grasses use to fertilize new seeds for growth. A pollen count is the number of grains of plant pollen per cubic meter, usually measured over a 24-hour period. Most weather forecasts feature pollen counts that can give you a rough estimate of daily allergy hazards, so pay attention to these and limit your time outdoors on days when the pollen counts soar. Pollen counts are also highest in the morning, so try to stay indoors until later in the day.
All material copyright MediResource Inc. 1996 – 2026. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Allergy-Prevention-and-Treatment
Nasal medications
Medication Management
Minor Ailments
Nasal medications (nose sprays) for allergies are available in a few different classes.
Nasal medications for allergies available in Canada include:
- non-prescription
- decongestants
- oxymetazoline (Dristan®, and others)
- xylometazoline (Balminil Nasal Decongestant®, Otrivin®, and others)
- corticosteroids
- fluticasone propionate (Flonase® and others)
- triamcinolone acetonide (Nasacort AQ®, Nasacort Allergy 24 HR®)
- prescription
- anticholinergics
- ipratropium (Atrovent Nasal Spray®)
- antihistamines
- levocabastine (Livostin Nasal Spray®)
- corticosteroids
- beclomethasone (Gen-Beclo AQ® and others)
- budesonide (Rhinocort Aqua® and others)
- ciclesonide (Omnaris®)
- fluticasone furoate (Avamys®)
- mometasone (Nasonex®)
Nasal decongestants provide temporary relief from congestion. However, they should not be used for more than 3 to 7 days because nasal congestion can return or get worse once you stop the medication. Since allergic rhinitis usually requires long-term treatment, it's best to talk to your doctor or pharmacist about which medication is right for you.
Antihistamines help relieve nasal itchiness, sneezing, and runny nose. They work by stopping the action of histamine, which is a substance in your body that causes an allergic response when you are exposed to an allergen. It is used 2 to 4 times a day. Side effects may include nasal irritation, drowsiness, nosebleeds, dry mouth, and headaches.
Anticholinergics are used to relieve a runny nose associated with allergies. They work by blocking the secretion of mucous in the nose. It is used 2 or 3 times a day. Side effects may include headaches, nosebleeds, nasal irritation, dry nose, and sore throat.
Corticosteroids are used to help relieve the symptoms of allergic rhinitis, including itching, congestion, runny nose, and sneezing. They work by locally reducing inflammation in the nose that is involved in an allergic reaction. The dosing of corticosteroids is once or twice a day, depending on the medication selected. Side effects of corticosteroids may include burning, stinging, nasal irritation, headaches, nosebleeds, sore throat, changes in taste, and dry mouth.
Each person may respond differently to medications and not everyone experiences the same side effects. If side effects are a concern for you, talk to your doctor about which nasal spray would best suit you.
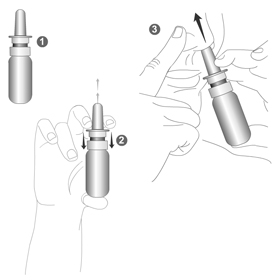
To use the nasal spray:
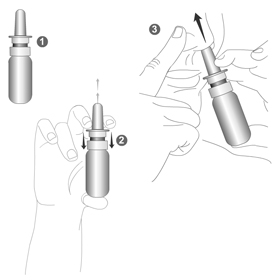
- First, gently blow your nose.
- Wash your hands well with soap and water.
- You may need to prime the nasal spray pump first by spraying it a few times into the air until a fine mist appears.
- Keep your head upright or tilted slightly forward.
- Use the "opposite hand to opposite nostril" technique. With your right hand, spray the medication into the left nostril toward the outside of the nose. Remember to breathe in deeply through your nose as you pump the spray.
- Repeat for the other nostril.
- Put the cap back on the nasal spray container.
- Wait a few minutes before blowing your nose.
- For more detailed instructions, see the package insert for your particular medication or check with your doctor or pharmacist.
People with certain medical conditions should not take some of these nasal medications. To ensure you are taking the most appropriate medication, inform your doctor and pharmacist of any other medications you are taking and of any medical conditions you have.
You should follow your doctor's and pharmacist's instructions on using the medication to ensure you get the most benefit from it. If you are taking any of these medications and your allergy symptoms do not go away completely, talk to your doctor.
All material copyright MediResource Inc. 1996 – 2026. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Allergy-Prevention-and-Treatment
Eye drops
Medication Management
Minor Ailments
Eye drops used to treat allergies are specifically for eye symptoms such as red, itchy, and watery eyes.
Eye drops for allergies available in Canada include:
- non-prescription
- decongestants / vasoconstrictors
- naphazoline (Clear Eyes®, Refresh Redness Relief®, and others)
- oxymetazoline (Sinex®, and others)
- prescription
- antihistamines
- emedastine (Emadine®)
- ketotifen (Zaditor®)
- olopatadine (Pataday®)
- mast cell stabilizers
Antihistamine eye drops provide relief of eye symptoms (i.e., ocular symptoms) in a few minutes. Decongestant eye drops also work in about 5 to 10 minutes. The mast cell stabilizers take a few days to see their full effects.
Dosing for these medications is usually 2 to 4 times a day, depending on the type of eye drops used. Side effects may include burning, stinging, eye irritation, headache, and changes in taste. Eye infections can occur, especially if the eye drops are not used properly.
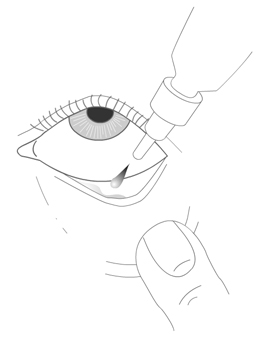
To use the eye drops:
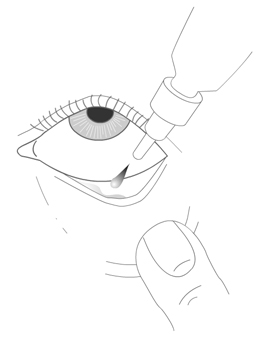
- First wash your hands thoroughly with soap and warm water. If you wear glasses or contact lenses, remove them.
- Tilt your head back, and with your eyes open, create a little pocket with your lower eyelid by pulling it away from the eye.
- Look up towards the ceiling, then squeeze the eye dropper gently to instill 1 drop into the pocket.
- Close your eyes, look down and apply gentle pressure to the corners of the eyes at the bridge of the nose to prevent the medication from draining into your tear duct. Try to keep your eye closed for at least 30 seconds.
- Repeat with the other eye, if applicable.
- Try not to touch the tip of the eye dropper onto your eye or any other surface.
- For more detailed instructions, see the package insert for your particular medication or check with your doctor or pharmacist.
People with certain medical conditions should not use some of these eye drops. To ensure you are taking the most appropriate medication, inform your doctor and pharmacist of any other medications you are taking and of any medical conditions you have.
You should follow your doctor's and pharmacist's instructions on using the medication to ensure you get the most benefit from it. If you are taking any of these medications and your allergy symptoms do not go away completely, talk to your doctor.
All material copyright MediResource Inc. 1996 – 2026. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Allergy-Prevention-and-Treatment
Oral medications
Medication Management
Minor Ailments
Oral medications (i.e., taken by mouth) for allergic rhinitis include antihistamines and decongestants.
Oral medications for allergies available in Canada include:
- non-prescription
- antihistamines
- cetirizine (Reactine® and others)
- chlorpheniramine (Chlor-Tripolon® and others)
- desloratadine (Aerius®)
- diphenhydramine (Benadryl® and others)
- fexofenadine (Allegra® and others)
- loratadine (Claritin® and others)
- antihistamine and decongestant combination products
- cetirizine - pseudoephedrine (Reactine® Allergy & Sinus)
- deslorataine - pseudoephedrine (Aerius® Dual Action)
- fexofenadine - pseudoephedrine (Allegra-D®)
- loratadine - pseudoephedrine (Claritin® Allergy & Sinus)
- triprolidine - pseudoephedrine (Actifed®)
- decongestants
- phenylephrine (Sudafed PE® and others)
- pseudoephedrine (Eltor®, Sudafed® and others)
- prescription
- antihistamines
- leukotriene receptor antagonists
Antihistamines work by stopping the action of histamine, which is a substance in your body that causes an allergic response when you are exposed to an allergen. Antihistamines reduce the symptoms of eye itching, nasal itching, runny nose, sneezing, and watery eyes, while oral decongestants help with nasal congestion. Desloratadine is an antihistamine that also relieves nasal congestion. Antihistamines and oral decongestants can be used together to relieve allergy symptoms.
The third type of oral allergy medications is leukotriene receptor antagonists (montelukast), which work by blocking leukotrienes. Leukotrienes are chemicals that are released by your body during an allergic response. They are also involved in causing allergy symptoms.
Side effects of oral medications
- The side effects of antihistamines may include dry mouth, constipation, drowsiness, difficulty urinating, and decreased reaction time. At normal recommended doses, cetirizine, desloratadine, fexofenadine, and loratadine have fewer side effects than other antihistamines.
- The side effects of decongestants include headache, dizziness, dry mouth, palpitations (rapid, irregular heartbeat), tremor, and trouble sleeping. Normal doses of oral decongestants can also increase the blood pressure in people who have high blood pressure. People who have severe or poorly controlled high blood pressure should not take oral decongestants.
- The most common side effects of montelukast include diarrhea, stomach pain, headache, thirst, itchy skin, and rash.
Some oral medications may affect people with certain medical conditions (including high blood pressure, glaucoma, and low thyroid) and may not be a suitable treatment option. To ensure that you are taking the most appropriate medication, inform your doctor and pharmacist of any other medications you are taking and any medical conditions you have.
You should follow your doctor's and pharmacist's instructions on taking the medication to ensure you get the most benefit from it. If you are taking any of these medications and your allergy symptoms do not go away completely, talk to your doctor.
All material copyright MediResource Inc. 1996 – 2026. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/healthfeature/gethealthfeature/Allergy-Prevention-and-Treatment